Dental Pain and Infection
Tell us where it hurts and we will make it go away!!!

Dental Pain is pain in the teeth, their supporting structures, or both; caused by dental disease or non-dental disease which is perceived as toothache. The most common cause is pulpitis (inflammation of the tooth pulp), usually as a result of dental decay or dental trauma; and its sequel, periapical periodontitis and periapical abscess (infection). Since the causes of toothache are varied, the treatment is dependent upon the exact cause.
Treatments available for Dental Pain and Infection are:
- ROOT CANAL TREATMENT
- ABSCESS DRAINAGE
- TOOTH REMOVAL
- LASER DISINFECTION – HELBO TREATMENT
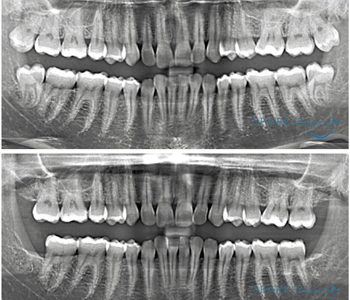
1. ROOT CANAL TREATMENT
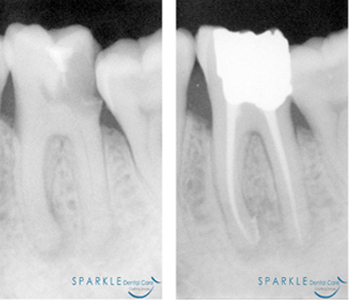
It's understandable you'd be concerned, maybe even scared, about the possibility of having a root canal procedure. Over the years, root canals have become synonymous with serious pain; but they've actually come a long way. New technology now enables us to perform the procedure virtually pain-free. And once the root canal procedure is complete, it's likely you'll be free of pain afterwards, too!
Root canal treatment is necessary when the pulp (soft tissue inside your teeth containing blood vessels, nerves and connective tissue) becomes inflamed or diseased. During root canal treatment, we remove the diseased pulp. The pulp chamber and root canal(s) of the tooth are then cleaned and sealed. If the infected pulp is not removed, pain and swelling can result, and your tooth may have to be removed.
If you continue to care for your teeth and gums your restored tooth could last a lifetime. However, regular checkups are necessary; a tooth without its nerve can still develop cavities or gum disease. Most of the time, a root canal is a relatively simple procedure with little or no discomfort involving one to three visits.
By saving your tooth, we can help you keep your natural smile, so you can continue to eat your favorite foods and maintain your overall health. Nothing looks, feels or functions like your natural tooth! Save your tooth, Save your smile. Speak with us; let us clear your doubts and help you know more about this procedure!!!
Back to top
SINGLE SITTING ROOT CANAL TREATMENT

Single Sitting Root Canal Treatment is one of the recent advances in the branch of endodontics. Previously, it was not highly recommended specially in non-vital teeth. But now, with revolutionary changes in concepts and availability of better equipment and materials, it is considered as a routine & painless procedure even in non-vital teeth. Single sitting Root Canal Treatment is now days extremely popular. We at SPARKLE DENTAL CARE perform Single Sitting Root Canal Treatment whenever the case permits! Speak with us; let us clear your doubts and help you know more about this procedure!!!
Back to top
RE-ROOT CANAL TREATMENT
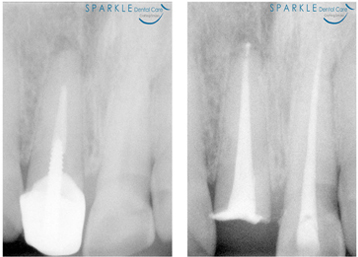
As occasionally happens with any dental or medical procedure, a tooth may not heal as anticipated after initial treatment for a variety of reasons:
- Narrow or curved root canals sometimes pose complications during the initial procedure.
- Complicated root canal anatomy (shapes and forms) went undetected in the first procedure.
- The placement of the crown or other restoration was delayed following the treatment, resulting in reinfection of the root canals.
- An inadequate seal of a restoration (filling) allowed recontamination of the inside of the tooth.
Some of these issues do not give rise to symptoms, but can give rise to chronic infection, often seen in an x-ray picture as a small black area around the end of an affected root. New problems too, can jeopardize a tooth that initially had successful root canal treatment; like:
- New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth.
- A loose, cracked or broken crown or filling can expose the tooth to new infection.
- A tooth sustains a fracture of the crown or root.
During re-treatment, all options will be reviewed, together with the risks, benefits and alternatives. Assuming the tooth can be retreated, it will need to be “reopened”. A small hole will be made into the biting or chewing surface of the tooth to gain access to the root canal. In many cases, crown, post and core material must be removed to permit access to the root canals. The previous root canal filling materials are removed and the canals cleaned and carefully examined, which includes searching for any additional canals or unusual canals that require treatment. After cleaning and shaping the canals they will be sealed and a temporary filling or crown placed. Upon successful completion and healing of infection, a new crown or restoration will need to be placed on the tooth to protect and restore it to its full form and function.
Whenever possible, it is best to save your natural tooth. Retreated teeth can function well for years. Advances in technology are constant and updated techniques may be used to save a tooth, which may not have been available when you had your first procedure. The only other alternative to retreatment or failing endodontics ultimately is extraction of the tooth. Speak with us; let us clear your doubts and help you know more about this procedure!!!
Back to top
2. ABSCESS DRAINAGE

A dental abscess is not to be taken lightly. This is a serious infection that can result in pain, loss of tooth or worse. An abscessed tooth is an infection caused by tooth decay, periodontal disease or a cracked tooth. These problems can let bacteria enter the pulp (the soft tissue of a tooth that contains nerves, blood vessels and connective tissue) and can lead to pulp death. When pus builds up at the root tip in the jaw bone, it forms a pus-pocket called an abscess. If the abscess is not treated, it can lead to a serious infection in the jaw bone, teeth and surrounding tissues. Symptoms of an abscess include pain, swelling, redness in the gums, bad taste in the mouth and fever.
An abscessed tooth can be treated with various treatments, depending on the severity of the infection. Here are some of the treatment methods we may have to consider:
- antibiotics, to destroy the bacteria causing the infection
- drainage of the infection
- cleaning the space between the tooth and the gum if the cause is from gum disease
- root canal treatment if the abscess is caused by decay or a cracked tooth
Following good oral hygiene practices and routine dental exams will significantly reduce your risk of developing a tooth abscess. If your teeth experience trauma (become loosened or chipped), see us as soon as possible. Speak with us; let us clear your doubts and help you know more about this procedure!!!
Back to top
3. TOOTH REMOVAL

An extraction means to have a tooth removed, usually because of disease, trauma or crowding. If you need an extraction, we first numb the area to lessen any discomfort. After the extraction, we will advise you of what post extraction regimen to follow. In most cases a small amount of bleeding is normal. Your mouth will slowly fill in the bone where the tooth root was through the formation of a blood clot.
Here are some tips to follow to make recovery easier:
- Avoid anything that might prevent normal healing.
- Don’t smoke or rinse your mouth vigorously.
- Avoid drinking through a straw for 24 hours.
- Follow the diet we suggest.
For the first few days, if you must rinse, rinse your mouth gently. If you experience swelling, apply a cold cloth or an ice bag and call us right away. You can brush and floss the other teeth as usual. But don't clean the teeth next to where the tooth was removed. Remember, when having an extraction, today's modern procedures and follow up care (as recommended by us) are there for your benefit and comfort. Speak with us; let us clear your doubts and help you know more about this procedure!!!
DISIMPACTION – WISDOM TOOTH REMOVAL
Wisdom teeth, also referred to as third molars, get their name by being the last teeth to come in during young adulthood. As part of a dental visit, we will examine you to determine if your wisdom teeth are healthy and properly positioned. Wisdom teeth due to certain developmental difficulties do not erupt in their right place. They often remain dormant inside the bone
Every patient is unique, but in general, wisdom teeth may need to be removed when there is evidence of changes in the mouth such as:
- pain
- foci of infection
- cysts
- tumors
- damage to adjacent teeth
- gum disease
- tooth decay (if it is not possible or desirable to restore the tooth)
- problem due to the forces they exert
We may also recommend removal to prevent problems or for others reasons, such as when removal is part of an orthodontic, restorative or periodontal treatment plan.
In addition, the condition of your mouth changes over time. Wisdom teeth that are not removed should continue to be monitored, because the potential for developing problems later on still exists. As with many other health conditions, as people age, they are at greater risk for health problems and that includes potential problems with their wisdom teeth. Regular dental visits are important so that we can evaluate not just your wisdom teeth but your overall oral health to help you prevent and manage dental disease and achieve optimal oral health.
When they need to be removed, we can easily help you. Speak with us; let us clear your doubts and help you know more about this procedure!!!
Back to top
4. LASER DISINFECTION – HELBO TREATMENT

Pathogenic bacteria are the main cause of failure in dentistry! Studies have shown that the biofilm provides a safe habitat for them. The more mature the biofilm, the more resistant the bacteria within it become. Mechanical cleaning and rinsing solutions do not adequately destroy the bacteria in the biofilm. Even strong antibiotics seldom provide sustainable success. There are, however, side effects, interactions with other medications and the risk of resistance when using antibiotics. Periodontal pathogenic bacteria increase the risk of numerous diseases like Periodontitis and periimplantitis; Endodontitis; Caries; Alveolar ostitis following tooth extraction; Bone necrosis; Inadequate healing following apicoectomy and Residual ostitis (disturbed healing of an implant, in particular in the case of immediate implantation).
With HELBO Treatment we can quickly relieve from these inflammations/infections or prevent disturbances to wound healing. The light also accelerates the healing process and has a proven analgesic effect. The proposed treatment is based upon the marking of the bacterial wall using light-sensitive dye molecules, which diffuse into the biofilm. The dye molecules are then activated using laser light and transfer their energy into local oxygen. This creates highly aggressive singlet oxygen, which destroys more than 99 percent of the bacteria in the biofilm. An efficacy rate as high as this would be unthinkable using conventional treatment methods. Speak with us; let us clear your doubts and help you know more about this procedure!!!
Back to top

